A Revolutionary Understanding of Maternal Mental Health
Picture this: You’ve just brought your beautiful baby home, but instead of pure joy, you’re drowning in unexplained sadness, anxiety, and overwhelming fatigue. If this sounds familiar, you’re not alone—and there might be a surprising explanation hiding in your gut.
Recent groundbreaking research reveals that the trillions of bacteria living in your digestive system may hold the key to understanding and treating postpartum depression (PPD). This isn’t just another wellness trend—it’s a scientific breakthrough that could transform how we approach maternal mental health.
The Reality of Postpartum Depression
Postpartum depression affects an estimated 10-15% of new mothers, making it one of the most common complications of childbirth. Yet despite its prevalence, PPD remains poorly understood and often undertreated.
Common symptoms include:
- Persistent sadness and mood swings
- Severe anxiety and panic attacks
- Difficulty bonding with your baby
- Overwhelming fatigue and sleep disturbances
- Loss of appetite or overeating
- Feelings of guilt, shame, or inadequacy
- In severe cases, thoughts of harming yourself or your baby
Traditional approaches focus on hormonal changes, sleep deprivation, and psychological factors. While these elements certainly play a role, emerging research suggests we’ve been missing a crucial piece of the puzzle: your gut microbiome.
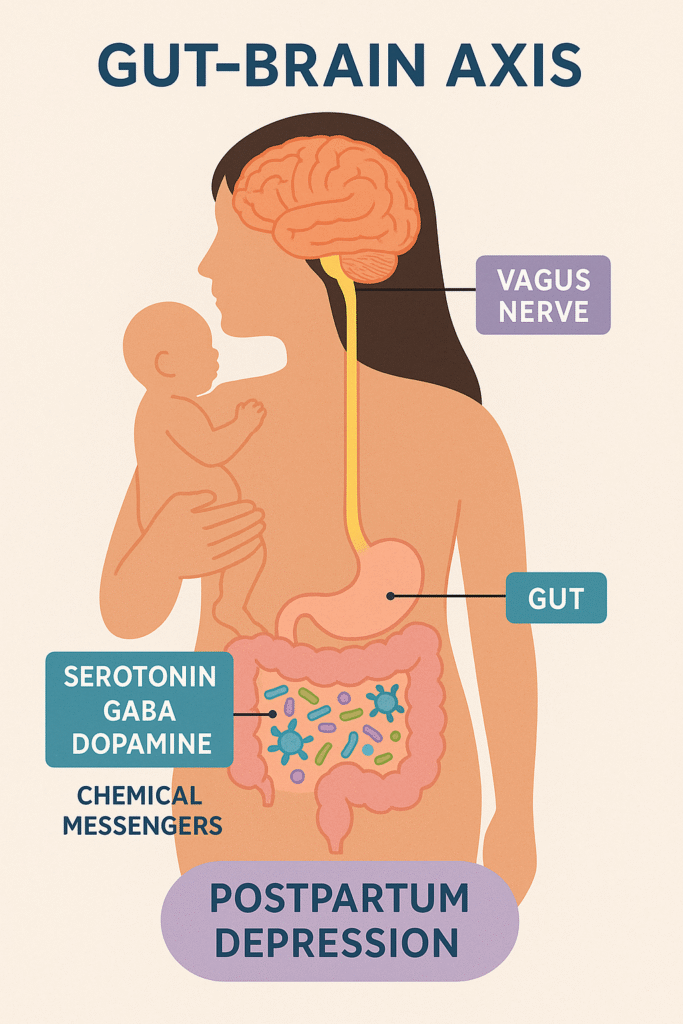
Your Second Brain: The Gut-Brain Highway
Your digestive system houses what scientists call the “enteric nervous system”—essentially a second brain containing more nerve cells than your spinal cord. This isn’t just poetic language; it’s biological reality.
The gut-brain axis operates through multiple communication channels:
Direct Neural Pathways
The vagus nerve acts as a superhighway, carrying signals between your gut and brain in both directions. When your gut bacteria are out of balance, these signals can trigger mood changes, anxiety, and depression.
Chemical Messengers
Your gut bacteria produce neurotransmitters—the same chemicals that regulate mood in your brain:
- Serotonin: 90% is produced in your gut
- GABA: The brain’s primary calming neurotransmitter
- Dopamine: Essential for motivation and pleasure
Hormone Production
Here’s where it gets really interesting: certain gut bacteria can actually produce hormones. Recent Harvard research discovered that specific bacterial strains (G. pamelaeae and E. lenta) can manufacture allopregnanolone—a neurosteroid directly linked to postpartum depression. The synthetic version of this compound, brexanolone, is currently FDA-approved for treating PPD.
Immune System Modulation
Your gut microbiome serves as mission control for your immune system. When bacteria are imbalanced, inflammation increases throughout your body, including your brain—a known contributor to depression.
The Perfect Storm: How Pregnancy Changes Everything
Pregnancy and childbirth create dramatic shifts in your body’s bacterial ecosystem. While some changes are necessary adaptations, others can set the stage for postpartum depression.
Normal Pregnancy Changes
During pregnancy, your microbiome naturally shifts to:
- Support fetal development
- Prepare for breastfeeding
- Manage increased nutritional demands
These changes include decreased butyrate-producing bacteria (like Faecalibacterium) and increased Proteobacteria and Bifidobacteria.
When Normal Becomes Problematic
The critical difference between healthy adaptation and disease-promoting dysbiosis appears to lie in the magnitude and duration of these changes. When bacterial shifts become excessive or prolonged, they cross the line from beneficial adaptation to pathological imbalance.
The Smoking Gun: Bacterial Imbalances in Postpartum Depression
Multiple studies have identified consistent patterns of gut dysbiosis in women with postpartum depression compared to healthy mothers.
The Depleted “Good Guys”
Women with PPD show significantly reduced levels of beneficial bacteria:
Faecalibacterium (9.22% vs. 19.79% in healthy controls)
- Produces butyric acid, a powerful anti-inflammatory compound
- Levels negatively correlate with depression severity
Lachnospiraceae family
- Major butyrate producers
- Associated with hormone regulation
Butyricicoccus
- Another butyrate producer
- Commonly depleted in inflammatory conditions
The Overgrown “Bad Guys”
Simultaneously, harmful bacteria flourish in PPD:
Enterobacteriaceae family
- Causes gut inflammation and “leaky gut”
- Promotes systemic inflammation
Escherichia-Shigella
- Positively correlated with depression severity
Enterococcus
- Associated with increased mood symptoms
This pattern reveals a critical theme: the butyrate-inflammation axis. Reduced production of anti-inflammatory butyrate, combined with increased inflammatory bacteria, creates a perfect storm for depression.
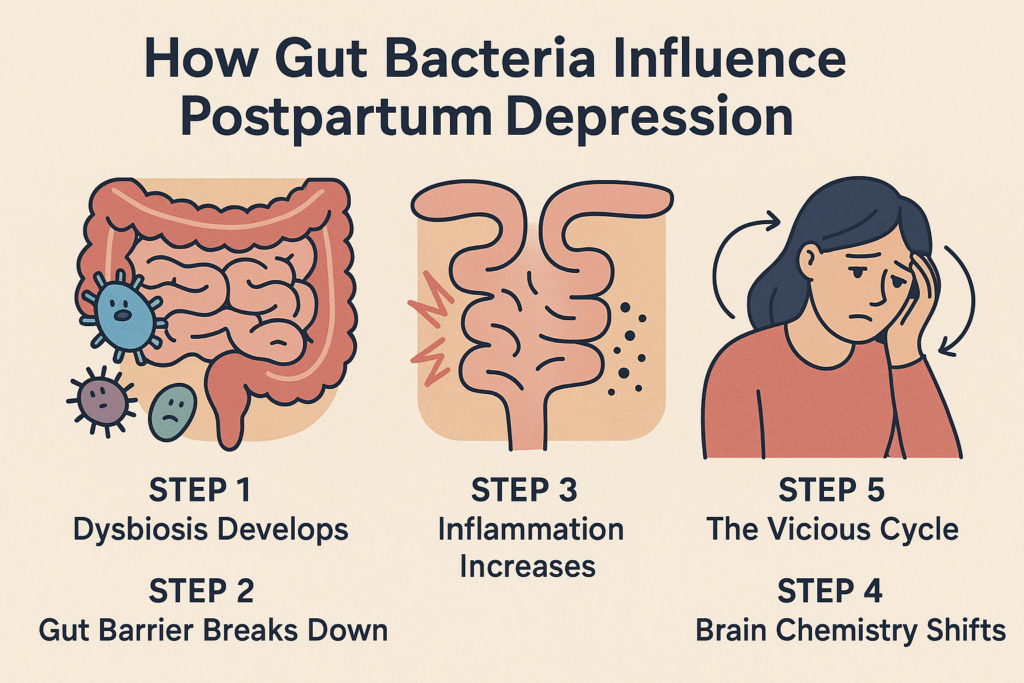
The Biological Cascade: From Gut to Mood
Understanding how gut bacteria influence postpartum depression requires following the biological breadcrumbs:
Step 1: Dysbiosis Develops
Factors like poor diet, stress, C-section delivery, or antibiotic use disrupt the bacterial balance.
Step 2: Inflammation Increases
Reduced beneficial bacteria mean less anti-inflammatory butyrate production, while pathogenic bacteria produce inflammatory compounds.
Step 3: Gut Barrier Breaks Down
“Leaky gut” allows inflammatory molecules to enter circulation, reaching the brain.
Step 4: Brain Chemistry Shifts
Neuroinflammation disrupts neurotransmitter production and hormone balance, triggering depression symptoms.
Step 5: The Vicious Cycle
Depression and stress further disrupt the gut microbiome, perpetuating the cycle.
Risk Factors That Wreck Your Gut
Several common experiences during pregnancy and postpartum can predispose you to gut dysbiosis and increase PPD risk:
Dietary Factors
- High-sugar, processed foods: Feed harmful bacteria and promote inflammation
- Low fiber intake: Starves beneficial bacteria
- Nutrient deficiencies: B vitamins, omega-3s, vitamin D, iron, magnesium, and zinc are all crucial for both gut health and mood regulation
Stress (The Silent Disruptor)
Maternal stress directly alters gut bacteria composition. Studies show that stressed mothers have:
- More pathogenic bacteria (Erwinia, Serratia, Bacteroides)
- Fewer beneficial strains (Lactococcus, Lactobacillus, Akkermansia)
Importantly, objective stress markers (like cortisol levels) show stronger associations with microbiome changes than self-reported stress, suggesting that even unconscious stress affects your gut.
Medical Interventions
- C-section delivery: Infants miss exposure to beneficial vaginal bacteria, starting life with a less diverse microbiome
- Antibiotic use: Dramatically reduces microbial diversity and can have lasting effects on both mother and baby
Hope on the Horizon: Gut-Targeted Treatments
The exciting news is that understanding the gut-brain connection opens entirely new treatment avenues for postpartum depression.
Probiotic Interventions
Research focuses on specific strains showing promise for mental health:
Currently Being Studied:
- Lactobacillus paracasei 431
- Bifidobacterium lactis BB-12
- Lactobacillus rhamnosus HN001
Important Note: Probiotic effectiveness is highly strain-specific. Not all probiotics are created equal, and more research is needed to identify optimal strains and dosages for PPD.
Nutritional Strategies
A comprehensive approach includes:
Prebiotic Foods (feed beneficial bacteria):
- Artichokes, garlic, onions
- Asparagus, bananas
- Oats, flaxseeds
Fermented Foods (provide live beneficial bacteria):
- Yogurt with live cultures
- Kefir, sauerkraut, kimchi
- Miso, tempeh
Anti-inflammatory Nutrients:
- Omega-3 fatty acids (fatty fish, walnuts, flaxseeds)
- Vitamin D (sunlight, fortified foods, supplements)
- Magnesium (dark leafy greens, nuts, seeds)
- Zinc (meat, legumes, pumpkin seeds)
Lifestyle Interventions
Stress Management Techniques:
- Mindfulness meditation (proven to alter gut bacteria composition)
- Yoga and gentle exercise
- Deep breathing exercises
- Social support networks
These approaches work by activating the parasympathetic nervous system, which supports both gut health and mental well-being.
The Future of Maternal Mental Health
We’re standing at the threshold of a new era in postpartum depression treatment. Future developments may include:
Personalized Microbiome Medicine
Instead of one-size-fits-all treatments, doctors might analyze your specific bacterial profile to prescribe targeted interventions.
Microbiome-Based Biomarkers
Simple stool tests could identify PPD risk before symptoms appear, enabling preventive interventions.
Novel Therapeutic Approaches
Understanding that gut bacteria can produce mood-regulating hormones opens possibilities for bacterial “hormone factories” as treatments.
Practical Steps You Can Take Today
While research continues, you can start supporting your gut-brain health immediately:
During Pregnancy
- Eat a diverse, fiber-rich diet with plenty of fruits, vegetables, and whole grains
- Include fermented foods regularly (at least 3 servings per week)
- Manage stress through meditation, yoga, or counseling
- Discuss antibiotic use carefully with your healthcare provider
- Consider prenatal probiotics (consult your doctor first)
Postpartum
- Prioritize nutrition despite exhaustion—meal prep and support systems are crucial
- Stay hydrated to support gut motility
- Gradually reintroduce exercise to promote beneficial bacteria
- Seek social support to buffer stress effects
- Monitor your mental health and don’t hesitate to seek help
Red Flags to Watch For
Seek immediate professional help if you experience:
- Thoughts of harming yourself or your baby
- Inability to care for yourself or your infant
- Severe anxiety or panic attacks
- Complete loss of interest in your baby
A Message of Hope
If you’re struggling with postpartum depression, remember that it’s not your fault, and it’s not a reflection of your ability as a mother. Your gut bacteria don’t define you, but understanding their role can empower you to take control of your recovery.
The connection between gut health and postpartum depression represents more than just scientific curiosity—it’s a pathway to hope. By addressing the root causes of dysbiosis through nutrition, stress management, and targeted interventions, we can potentially prevent and treat this devastating condition more effectively than ever before.
Your journey to mental wellness might just begin in your gut. And that’s not just hopeful thinking—it’s science.
Remember: This information is educational and doesn’t replace professional medical advice. Always consult healthcare providers for personalized guidance, especially if you’re experiencing postpartum depression symptoms.